Abstract
Introduction: Chemotherapy-induced peripheral neuropathy (CIPN) is a common adverse effect of cancer therapy seen with platinum agents, taxanes, vinca alkaloids, and proteasome inhibitors that can have a profound and lasting impact on quality of life. Although recognized during treatment with dose reductions and pain management, there may be an opportunity for a more uniform approach to help reduce the severity and enhance recovery. Our interdisciplinary team developed a clinical pathway and educational tool for managing neuropathy in patients who received systemic antineoplastic therapy. The gynecologic oncology team developed the pathway that now will be used in the hematologic malignancy team, especially for our patients with lymphoid malignancies who also often experience CIPN.
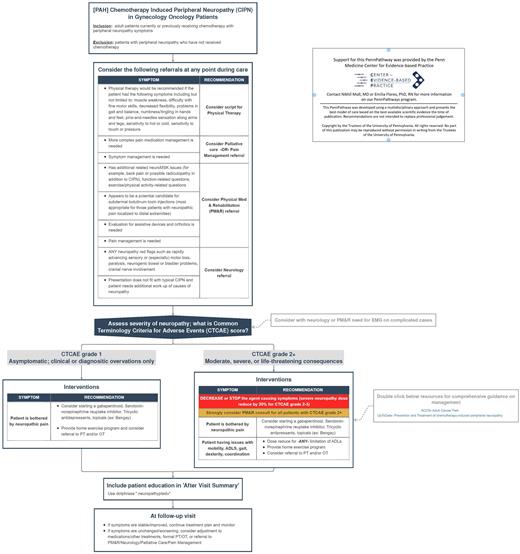
Methods: A multidisciplinary team of specialists, including physicians, advanced practice providers, nurses, and social workers from gynecologic oncology, medical oncology, physical medicine and rehabilitation (PM&R), and physical and occupational therapy (PT/OT), was convened. A literature review was performed to collate evidence-based practices for neuropathy management. The review informed the development of the clinical pathway and led to the creation of provider-facing and patient-facing materials. Dissemination and access to the pathway included uploading a schematic onto a shared health system clinical care platform (Dorsata). The tool provides clinical decision support to providers by standardizing the approach to triage, navigation, and multi-modality neuropathy treatment. The pathway structure is based on symptoms' severity and includes social needs. Implementation included clinical decision support built within the electronic medical records platform (EPIC) using smart phrases. These interventions facilitated PMR, PT/OT, Neurology & Palliative Care referrals. Simultaneously, patient-facing materials were also made accessible through EPIC. The content included the causes of neuropathy, interventions for management, and injury prevention. Armed with this knowledge, we aim to empower patients in understanding and taking control of their symptoms.
Results: There have been 35 views since the pathway was published in April 2022. This pathway increased clinician recognition of neuropathy as a highly prevalent and burdensome side effect of antineoplastic therapy. The standardized pathway allowed the entire treatment team to facilitate care easily and without added time. Patients were highly interested in strategies to ameliorate neuropathy symptoms and learned that multi-modality treatment options are available. Feedback from the pilot process thus far has resulted in plans to: (1) utilize a nurse navigator and clinical nurses to assist in triaging patients through this clinical care pathway, (2) collect validated neuropathy assessments pre and post-multimodal intervention, (3) expand to all oncology services lines within the health system.
Conclusion: We developed and piloted a clinical care pathway to manage neuropathy by leveraging expertise from a multidisciplinary team of oncology-centered providers. Preliminary results suggest it improved provider-based recognition, treatment for neuropathy, strong patient interest, and satisfaction for improved access to multi-modality neuropathy treatment.
Disclosures
Ko:Tesaro: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal